HYGIENE AND INFECTION CONTROL POLICY
1. Purpose
2. Values
3. Scope
4. Background
5. Definitions
6. Hand Hygiene & Hand washing procedure
7. Requirements for clinical glove use
8. Hand care
9. Jewellery and fingernails
9.1 Jewellery
9.2 Fingernails
10. Drying hands after hand hygiene
11. Promoting client, visitor and volunteer hand hygiene
Review details
Appendices
Appendix 1: Hand washing procedure
1. Purpose
This policy will provide guidelines for procedures to be implemented at Seddon Therapies to ensure:
• effective and up-to-date control of the spread of infection
• the provision of an environment that is safe, clean and hygienic.
2. Values
Seddon Therapies is committed to protecting all persons from disease and illness by minimising the potential for infection through:
• implementing and following effective hygiene practices
• implementing infection control procedures to minimise the likelihood of cross-infection and the spread of infectious diseases and illnesses
• informing staff, volunteers and clients on the importance of adhering to the Hygiene Policy to maintain a safe environment for all users, and communicating the shared responsibility between all involved in the operation of Seddon Therapies.
3. Scope
This policy applies to the staff, volunteers, clients and others attending the premises of Seddon Therapies, including during offsite visits and activities.
4. Background
A person with an infection may or may not show signs of illness and, in many instances, the infectious phase of the illness may be in the period before symptoms become apparent, or during the recovery phase. While it is not possible to prevent all infections, businesses can prevent or control the spread of many infectious diseases by adopting simple hygiene practices.
An infection can be spread when an infected person attends the business premises and contamination occurs. A business can contribute to the spread of an infection through poor hygiene practices that allow infectious organisms to survive or thrive in the business environment.
The implementation of appropriate hygiene and infection control procedures aims to break the cycle and prevent the spread of infections at every stage. The National Health and Medical Research Council (NHMRC) suggest that to reduce illness in care giving, the three most effective methods of infection control are:
• effective hand washing
• exclusion of sick staff and clients
• immunisation.
Other strategies to prevent infection include:
• proper cough etiquette as per World Health Organisation Guidelines
• appropriate use of gloves
• effective cleaning of the business environment.
The NHMRC suggests that if these strategies are not implemented, all other procedures described in the business’s Hygiene Policy will have reduced effectiveness in preventing the spread of infection and illness.
5. Definitions
The terms defined in this section relate specifically to this policy.
Alcohol-based hand rub (ABHR): An alcohol-containing preparation designed for application to the hands in order to reduce the number of viable micro-organisms with maximum efficacy and speed.
Antiseptic hand wash: Antiseptic containing preparation designed for frequent use. It reduces the number of micro-organisms on intact skin to an initial baseline level after adequate washing, rinsing and drying. It is broad spectrum, fast acting and, if possible, persistent.
Cleaning: A process that removes visible contamination such as food waste, dirt and grease from a surface. This process is usually achieved by the use of water and detergent. During this process, micro-organisms will be removed but not destroyed.
Hygiene: The principle of maintaining health and the practices put in place to achieve this.
Infectious disease: A disease that can be spread, for example, by air, water or interpersonal contact.
Sanitising: A process that destroys micro-organisms. Sanitising a surface can reduce the number of micro-organisms present. The process of sanitisation usually involves ensuring a surface is thoroughly cleaned with both heat and water, followed by the use of chemicals.
Plain liquid soap: Detergents that do not contain antimicrobial agents or contain low concentrations of antimicrobial agents that are effective solely as preservatives. Plain liquid soaps should be pH neutral (pH 5.5 to 7).
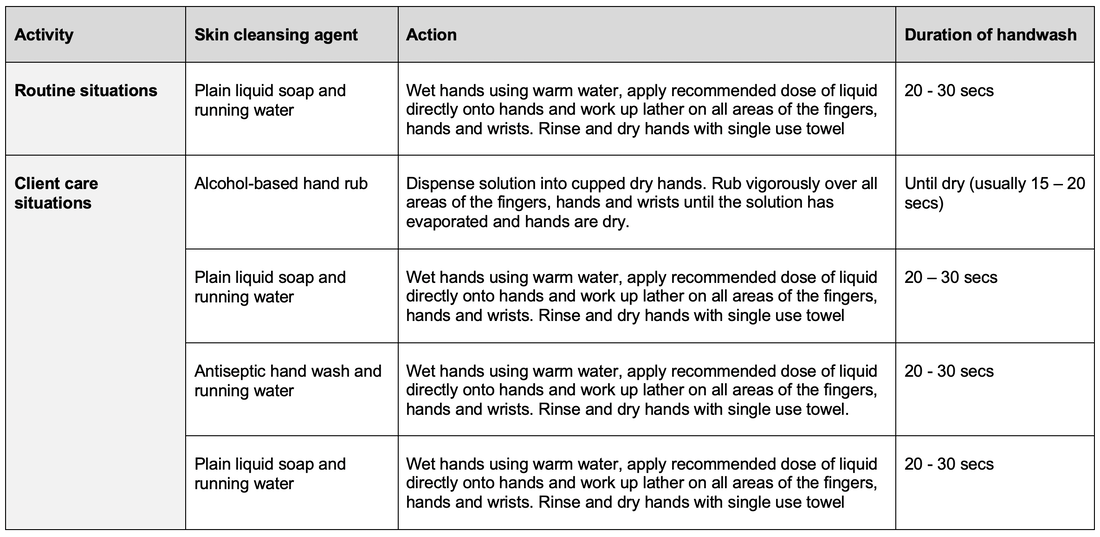
6. Hand hygieneHand washing procedure
Please see Appendix 1: Hand washing procedure.
7. Drying hands after hand hygiene
After cleansing hands, they must be dried before touching a client or commencing a procedure. Residual moisture left on the hands may harbour bacteria.
a. ABHR - continue rubbing hands vigorously until the ABHR has evaporated
b. Antiseptic hand wash/plain liquid soap – dry using single-use towels
c. Plain liquid soap – dry using single-use towels
Hot air hand dryers are not recommended.
8. Promoting client, visitor and volunteer hand hygiene
Therapists and other staff must encourage clients to perform hand hygiene and provide education on the correct hand hygiene technique. Clients should be provided with the means to perform hand hygiene at all times especially including after going to the toilet and coughing and sneezing.
Visitors and volunteers must perform hand hygiene at the point of care. Where visitors are likely to have physical contact with more than one client, then they must be encouraged to perform hand hygiene between clients.
9. Requirements for clinical glove use
Wearing gloves does not eliminate the need for hand hygiene. Therapists must:
a. Wear gloves when contact with body fluids is anticipated.
b. Change gloves during client care if moving from a contaminated body site to a clean body site.
c. Remove gloves after caring for a client.
d. Not wear the same pair of gloves for the care of more than one client.
e. Change and discard gloves if they become torn, punctured or compromised in any way.
f. Not sanitize, wash or reuse gloves.
g. Refer to the current infection control policy on personal protective equipment for further information about glove use from Department of Health and Human Services and World Health Organisation..
10. Hand care
It is important to ensure that the selected ABHRs, antiseptic hand washes, surgical hand scrubs and moisturising lotions are chemically compatible and pH neutral (5.5 to 7), to minimise skin reactions and to ensure that the decontaminating properties of the hand hygiene product are not deactivated.
If therapists experience hand care problems such as dryness, dermatitis and/or sensitivity, they should be reported to the manager.
The manager must ensure an alternative product is made available to therapists where sensitivity or allergy to these products is evident.
Therapists who have cuts and abrasions on exposed skin should consult with their manager. Possible solutions may include, but are not limited to use of gloves or “second skin” products.
11. Jewellery and fingernails
11.1 Jewellery
Several studies have shown that skin underneath rings is more heavily colonised than comparable areas of skin on fingers without rings. Wearing of rings in clinical areas by therapists must be limited to a plain band on the finger and this must be moved about on the finger during hand hygiene.
Other hand, wrist or forearm jewellery must not be worn by therapists providing direct client care unless required for client care (eg. watch) or are medically essential (eg. medical alert bracelet). These must be removable and able to be cleaned.
11.2 Fingernails
a. Nail polish must not be worn by therapists providing direct client care. Chipped nail polish supports the growth of larger numbers of organisms on the fingernails.
b. Artificial nails must not be worn by therapists providing direct client care. A growing body of evidence suggests that wearing artificial nails may contribute to the transmission of certain healthcare associated microorganisms.
c. Natural nail tips must be less than 0.6 centimetres (1/4 inch) long. Whether the length of the nail is a substantial risk is unknown however, long sharp fingernails can puncture gloves.
d. Nail art and technology must not be worn. There is limited information about nail art and technology but they may be a potential reservoir of microorganisms.
Review details
This policy was adopted by Seddon Therapies on 1st January 2020
This policy was last updated on 1st September 2020.
AppendicesAppendix 1: Hand washing procedure
2. Values
3. Scope
4. Background
5. Definitions
6. Hand Hygiene & Hand washing procedure
7. Requirements for clinical glove use
8. Hand care
9. Jewellery and fingernails
9.1 Jewellery
9.2 Fingernails
10. Drying hands after hand hygiene
11. Promoting client, visitor and volunteer hand hygiene
Review details
Appendices
Appendix 1: Hand washing procedure
1. Purpose
This policy will provide guidelines for procedures to be implemented at Seddon Therapies to ensure:
• effective and up-to-date control of the spread of infection
• the provision of an environment that is safe, clean and hygienic.
2. Values
Seddon Therapies is committed to protecting all persons from disease and illness by minimising the potential for infection through:
• implementing and following effective hygiene practices
• implementing infection control procedures to minimise the likelihood of cross-infection and the spread of infectious diseases and illnesses
• informing staff, volunteers and clients on the importance of adhering to the Hygiene Policy to maintain a safe environment for all users, and communicating the shared responsibility between all involved in the operation of Seddon Therapies.
3. Scope
This policy applies to the staff, volunteers, clients and others attending the premises of Seddon Therapies, including during offsite visits and activities.
4. Background
A person with an infection may or may not show signs of illness and, in many instances, the infectious phase of the illness may be in the period before symptoms become apparent, or during the recovery phase. While it is not possible to prevent all infections, businesses can prevent or control the spread of many infectious diseases by adopting simple hygiene practices.
An infection can be spread when an infected person attends the business premises and contamination occurs. A business can contribute to the spread of an infection through poor hygiene practices that allow infectious organisms to survive or thrive in the business environment.
The implementation of appropriate hygiene and infection control procedures aims to break the cycle and prevent the spread of infections at every stage. The National Health and Medical Research Council (NHMRC) suggest that to reduce illness in care giving, the three most effective methods of infection control are:
• effective hand washing
• exclusion of sick staff and clients
• immunisation.
Other strategies to prevent infection include:
• proper cough etiquette as per World Health Organisation Guidelines
• appropriate use of gloves
• effective cleaning of the business environment.
The NHMRC suggests that if these strategies are not implemented, all other procedures described in the business’s Hygiene Policy will have reduced effectiveness in preventing the spread of infection and illness.
5. Definitions
The terms defined in this section relate specifically to this policy.
Alcohol-based hand rub (ABHR): An alcohol-containing preparation designed for application to the hands in order to reduce the number of viable micro-organisms with maximum efficacy and speed.
Antiseptic hand wash: Antiseptic containing preparation designed for frequent use. It reduces the number of micro-organisms on intact skin to an initial baseline level after adequate washing, rinsing and drying. It is broad spectrum, fast acting and, if possible, persistent.
Cleaning: A process that removes visible contamination such as food waste, dirt and grease from a surface. This process is usually achieved by the use of water and detergent. During this process, micro-organisms will be removed but not destroyed.
Hygiene: The principle of maintaining health and the practices put in place to achieve this.
Infectious disease: A disease that can be spread, for example, by air, water or interpersonal contact.
Sanitising: A process that destroys micro-organisms. Sanitising a surface can reduce the number of micro-organisms present. The process of sanitisation usually involves ensuring a surface is thoroughly cleaned with both heat and water, followed by the use of chemicals.
Plain liquid soap: Detergents that do not contain antimicrobial agents or contain low concentrations of antimicrobial agents that are effective solely as preservatives. Plain liquid soaps should be pH neutral (pH 5.5 to 7).
6. Hand hygieneHand washing procedure
Please see Appendix 1: Hand washing procedure.
7. Drying hands after hand hygiene
After cleansing hands, they must be dried before touching a client or commencing a procedure. Residual moisture left on the hands may harbour bacteria.
a. ABHR - continue rubbing hands vigorously until the ABHR has evaporated
b. Antiseptic hand wash/plain liquid soap – dry using single-use towels
c. Plain liquid soap – dry using single-use towels
Hot air hand dryers are not recommended.
8. Promoting client, visitor and volunteer hand hygiene
Therapists and other staff must encourage clients to perform hand hygiene and provide education on the correct hand hygiene technique. Clients should be provided with the means to perform hand hygiene at all times especially including after going to the toilet and coughing and sneezing.
Visitors and volunteers must perform hand hygiene at the point of care. Where visitors are likely to have physical contact with more than one client, then they must be encouraged to perform hand hygiene between clients.
9. Requirements for clinical glove use
Wearing gloves does not eliminate the need for hand hygiene. Therapists must:
a. Wear gloves when contact with body fluids is anticipated.
b. Change gloves during client care if moving from a contaminated body site to a clean body site.
c. Remove gloves after caring for a client.
d. Not wear the same pair of gloves for the care of more than one client.
e. Change and discard gloves if they become torn, punctured or compromised in any way.
f. Not sanitize, wash or reuse gloves.
g. Refer to the current infection control policy on personal protective equipment for further information about glove use from Department of Health and Human Services and World Health Organisation..
10. Hand care
It is important to ensure that the selected ABHRs, antiseptic hand washes, surgical hand scrubs and moisturising lotions are chemically compatible and pH neutral (5.5 to 7), to minimise skin reactions and to ensure that the decontaminating properties of the hand hygiene product are not deactivated.
If therapists experience hand care problems such as dryness, dermatitis and/or sensitivity, they should be reported to the manager.
The manager must ensure an alternative product is made available to therapists where sensitivity or allergy to these products is evident.
Therapists who have cuts and abrasions on exposed skin should consult with their manager. Possible solutions may include, but are not limited to use of gloves or “second skin” products.
11. Jewellery and fingernails
11.1 Jewellery
Several studies have shown that skin underneath rings is more heavily colonised than comparable areas of skin on fingers without rings. Wearing of rings in clinical areas by therapists must be limited to a plain band on the finger and this must be moved about on the finger during hand hygiene.
Other hand, wrist or forearm jewellery must not be worn by therapists providing direct client care unless required for client care (eg. watch) or are medically essential (eg. medical alert bracelet). These must be removable and able to be cleaned.
11.2 Fingernails
a. Nail polish must not be worn by therapists providing direct client care. Chipped nail polish supports the growth of larger numbers of organisms on the fingernails.
b. Artificial nails must not be worn by therapists providing direct client care. A growing body of evidence suggests that wearing artificial nails may contribute to the transmission of certain healthcare associated microorganisms.
c. Natural nail tips must be less than 0.6 centimetres (1/4 inch) long. Whether the length of the nail is a substantial risk is unknown however, long sharp fingernails can puncture gloves.
d. Nail art and technology must not be worn. There is limited information about nail art and technology but they may be a potential reservoir of microorganisms.
Review details
This policy was adopted by Seddon Therapies on 1st January 2020
This policy was last updated on 1st September 2020.
AppendicesAppendix 1: Hand washing procedure